If you can produce small structures on a chip that can handle light, then suddenly all sorts of things become possible. For instance, a whole range of devices are used in medicine that examine cells, molecules and fibers with the help of fluorescent light. And now, thanks to photonics-on-chip, mini-versions of those same large devices can also be produced.
What is biophotonics-on-chip?
Chances are, you use photonics every day without even realizing it: glass fibers enable you to use a computer or watch television without any problems. With the help of light, these glass fibers send data much more quickly and power efficient than with traditional digital cables.
You can also do the same thing on a chip. Using ultra-small ‘fibers’ and structures, you can direct light on to a chip and carry out a whole range of tasks. Those tasks can involve processing or sending data, but biological tasks are also possible. In fact, light is the most frequently used medium in medical diagnostics – just think of microscopes and spectroscopes. Light enables you to count or visualize cells, measure the properties of materials and tissue, define a DNA sequence, etc.
Biophotonics-on-chip is a fairly recent area of research that is becoming very important in the medical sector for diagnosis, treatment and follow-up. Doctors will soon be able to use the technology to analyze a blood sample without bulky (fluorescence) microscopes, as well as examine a tissue sample without large spectroscopes.
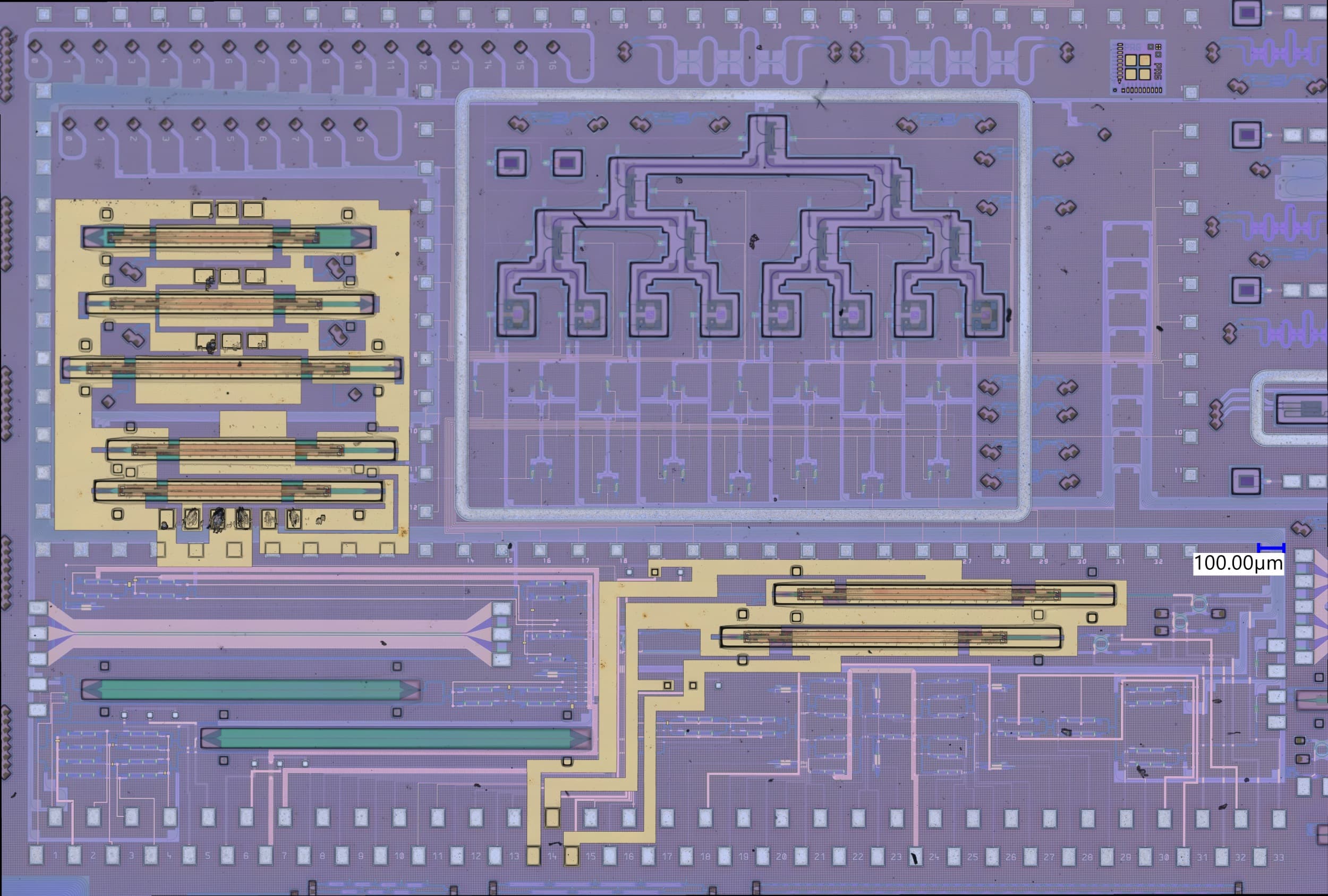
It is quite a challenge to make photonic structures very small and then combine them into a photonic circuit capable of carrying out a specific task with great efficiency and reliability. If you produce structures using silicon, such as computer chips, or based on silicon-compatible materials (SiN), you can incorporate electronic and photonic functions, creating a smart and compact system. And if you can do that, you can easily make hundreds and thousands of systems function alongside each other at the same time, which means you’ll also get the result much faster than with a single system on its own. Thanks to biophotonics-on-chip we will soon have small, cheap test chips that will assist doctors in their decisions.
Small ‘fibers’ of silicon nitride (SiN) are produced on top of a silicon chip. These waveguides direct the light along a well-defined path over the chip and along detection sites.
Some of the photonic components made by imec: spectrometer, fiber waveguide, waveguide and multi-mode interferometer.
Counting and viewing cells
Fluorescent labels are often used to analyze a blood sample in the traditional way. These labels are in fact molecules that bind specifically with, for example, (parts of) a bacterium, gene, cancer cell, etc. Using a cytometer, the blood sample and hence also the labels are illuminated, making them radiate fluorescent light that can be detected. This enables the number of bacteria and cancer cells to be counted or the presence of a specific gene or DNA sample to be determined.
Usually, cytometers are very large and expensive devices that are used in medical laboratories. Imec is developing more compact solutions: cytometers on a chip. In these chips, the cells flow in a microfluidic channel and there are structures above and/or below this channel for identifying and counting specific cells – for example cells with a fluorescent label.
A recent development in this area is a photonic structure called a ‘focusing grating coupler’. A grating coupler is usually used to couple the light coming from a laser (which shines on the chip) in the waveguide paths on the chip and to shine the light coming out of the waveguides back from the chip (e.g. to a detector that is not integrated on a chip). In the new development, the focusing grating coupler allows light, moving in a waveguide, to shine outward from the surface, to create an upward beam of light on top of the chip. The microfluidic channel that the cells flow along runs through this light beam. In this way, the cells with fluorescent labels are illuminated, after which they emit fluorescent light. This fluorescent light is captured by the ‘diffraction gratings’, which sort the light by wavelength. As a result, various fluorescent labels can be detected at the same time. This is a very good example of how compact photonic chips can be used to count cells, even different types of cells (with different fluorescent labels) at the same time. The big advantage of this approach is not so much that the cell can be optically detected, but that hundreds of these structures can work in parallel, having a huge impact on the throughput of these measurements.
Focusing grating couplers can send the light in waveguides outward from the surface, enabling them to efficiently illuminate the cells in the microfluidic channel located above.
Not only is it of value for counting cells, but it is also good for looking at the morphology of the cells. Here again imec has developed an integrated solution: the lens-free microscope. Read more about this in a previous article of imec magazine.
Spectroscopy in miniature
Spectroscopy is used in medicine to detect certain substances in tissue, skin or areas of the brain, such as cholesterol, lactic acid and ethanol. Melamine in milk, phthalate in toys, contamination in meat or the authenticity of medical drugs can also be detected with spectroscopy. The substances are detected by their specific interaction with wavelengths of light.
There are many forms of spectroscopy, including absorption, reflection, fluorescence and Raman spectroscopy. Imec is aiming to develop a mini-version of the Raman spectrometer on a chip. This would enable a compact little device to be produced for measuring specific substances in a blood sample regularly and non-invasively. This is not possible with existing desktop Raman spectrometers.
The major challenge in developing a Raman spectrometer is balancing the very small usable signal against the large background signal. That’s why the detector has to be very sensitive. One of the best-known spectrometer designs is the Michelson interferometer. A beam of light is divided into two beams that take different paths before coming together and interfering. This enables tiny differences in the wavelength to be measured. The disadvantage of this design – particularly if you want to miniaturize it – is that two mirrors are used, one of which moves. Unless the moving mirror is in absolutely the correct position, the measurement is incorrect.
Imec has developed a (patented) solution with no moving parts in which hundreds of structures – interferometers – are used next to each other. Light is shone on the tissue and the scattered light is collected by a collimator. This divides the light – with the help of a beam-shaper – across the various interferometers. Each interferometer is a little smaller than the previous one so that tiny differences in wavelengths can also be measured, as is the case with the Michelson interferometer.
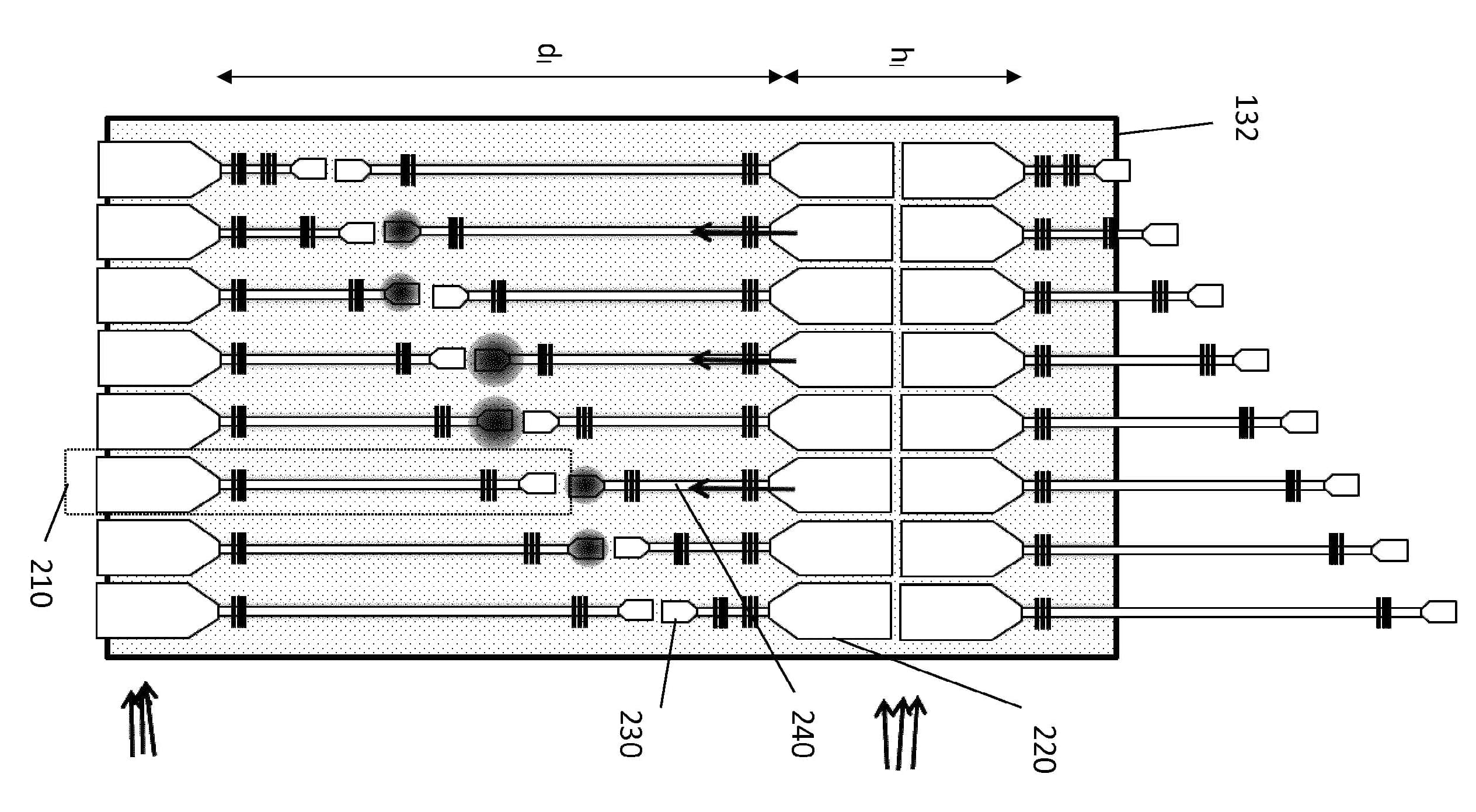
Design of the Raman spectrometer on chip.
A hypersensitive sensor based on light & sound
Photoacoustics is a fast, relative cheap and harmless way of producing images of the human body. It can be used, for example, in research into skin and breast cancer.
The photoacoustic effect was discovered in 1880 by Alexander Graham Bell, the inventor of the telephone. He illuminated a block of selenium, which created a weak sound (hence photo = light and acoustics = sound). In fact, light and sound are both forms of vibration. It’s just that we can’t ‘hear’ light, although it can be converted into sound.
With photoacoustics, very brief laser pulses are directed at the patient’s body. A different color of light is chosen, depending on the tissue. When one of these pulses touches the tissue, it is converted into heat. The tissue expands and then contracts again, creating a change in pressure, which moves again as ultrasound. This signal can be picked up by a sort of microphone. The ultrasound can be used to gather spectroscopic information about a material, or else it can be converted into an image. The big advantage of photoacoustics is that there is no background signal, which makes it a highly sensitive technique.
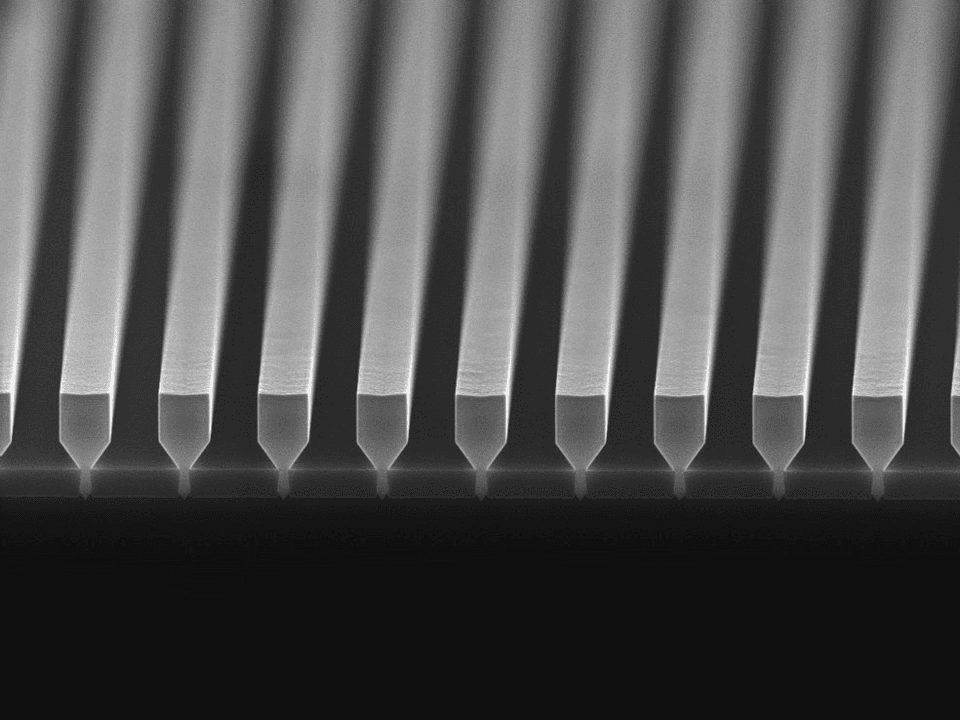
Photoacoustics are already used extensively in medical research, although not yet for diagnosing patients, because the technology is still too expensive. This is where imec aims to introduce a change by making a photoacoustic sensor on chip. One important component for this is the ‘microphone’, which must be able to pick up ultrasound. The ‘mic’ consists of a silicon oxide membrane with an integrated photonic waveguide. When the membrane moves under the pressure of a sound wave, the waveguide is stretched and this movement can be recorded.
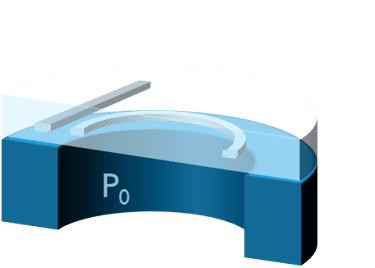
For its photoacoustic sensor-on-chip, imec uses a membrane with integrated waveguide. When the membrane is moved by a sound wave, the waveguide is stretched and this movement can be recorded.
Once it becomes possible to miniaturize spectrometers and photoacoustic sensors, the chip may be integrated in a pen like the one in the drawing. The doctor can then use the pen to scan the patient’s skin looking for disorders, such as skin cancer.
Want to try?
The PIX4life project began at the beginning of 2016. This is a European project, coordinated by imec, in which a ‘library’ of photonic components is being assembled. This library can then be used by companies – including SMEs – seeking to produce a medical application. By using multi-project wafers, the photonic chips can be produced more cheaply. The aim of the project partners is to lower the entry level for companies in order to take products featuring biophotonics more quickly to market. This will enable our doctors to have portable spectrometers, cytometers and microscopes sooner, meaning that the diagnosis of diseases and the follow-up of a revolutionary treatment can be improved.
Want to know more?
In this imec magazine read the article about a lab-on-chip that uses light to detect tuberculosis.
The PIX4life project is funded by the European Community as part of the Horizon 2020 research and innovation program (grant agreement nº 688519). More information at http://pix4life.eu.
Published on:
5 March 2017