Chris Van Hoof, imec fellow & Director Connected Health Solutions
In mid 2016, Bill Hait – global head of R&D at Johnson & Johnson Pharmaceutical Research and Development – said that the company’s long-term goal was to make significant progress towards a world without disease by 2030. His words heralded a trend that became visible in 2017: smart healthcare is shifting its focus from diagnostics and therapy to disease prevention and disease interception. While disease prevention mainly focuses on stimulating (healthy) behavior, disease interception implies capturing a disease before the first symptoms occur and developing therapies applicable in such an early stage of the disease process. Both prevention and disease interception require personal digital phenotyping – the use of digital and wearable technology to track health parameters and behavior over an extended period of time so as to identify risk factors and triggers. To turn this vision into reality, technology innovation is key.
Advancing the state-of-the-art: mobile and low-cost diagnostic solutions
At imec, wearable health R&D has traditionally focused on developing highly-comfortable, medical-grade wireless solutions for the diagnosis and management of cardiovascular, neurological and cardiopulmonary disorders. Our most recent wireless chest patch in 2017 combines ECG, respiration rate, respiration depth and actimetry. Due to its compact size and design, it significantly increases patients’ comfort and can be worn day or night to screen or diagnose. We are currently running clinical investigational studies to explore its potential use for patients with congestive heart failure and chronic kidney disorder.
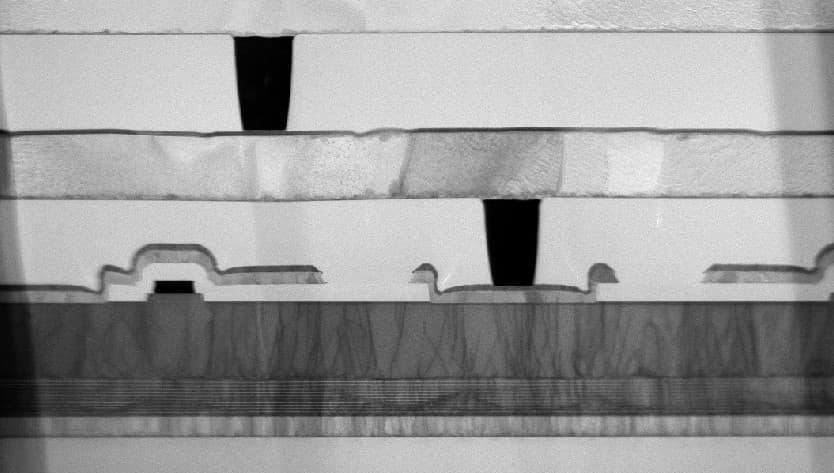
In 2017, we also completed a next generation of our MUSEIC chip, a low-power multi-(bio)sensor system-on-chip. It combines a wide range of on-chip electrophysiological sensor readouts with sensor fusion, powerful (yet ultra-low-power) signal processing, memory, power management, connectivity, and is at the same time equipped with built-in security and encryption. This platform can be used for very diverse diagnostic applications, but can also feature in smart watches and fitness trackers for wellness assessment. With such a complex system-on-chip, we can reduce the complexity at the system and application level. The new-generation MUSEIC chip could, for instance, be used to create a disposable single-use diagnostic smart Band-Aid that people could just buy at the pharmacy for prescribed diagnostic applications. This could significantly enhance chronic patients’ comfort and convenience. The expected cost reduction can also help to bring much needed chronic disease tools to developing countries.
Prevention through digital phenotyping: digital coaching for a healthy life
Providing accurate diagnosis and efficient treatment tools addresses an important need, but it would be even better if we could prevent people from becoming sick in the first place. That is why, in 2017, and after several years of preparation, we have set up the imec.ichange program, our first step towards a ‘world without disease’. According to the WHO, unhealthy behavior and lifestyle are at the root of nearly 80% of chronic diseases, which in turn are responsible for 60% of all deaths. Consequently, 70-85% of the healthcare budgets of OECD countries are spent treating chronic patients. This implies that true prevention has a tremendous potential to save lives and curb healthcare costs.
Digital phenotyping is one of the tools that we can use to prevent chronic disease. There are already a myriad of fitness trackers and sports watches that aim to motivate us to make healthier choices and try to make us fit, but their success rate is unclear: between thirty to fifty percent of users discard them after 6 months. One of the main reasons is that good intentions are short-lived if you only focus on maintaining motivation through simple metrics (steps, floors, heart rate) and generic advice.

To achieve a lasting behavior change, we need to go beyond motivation and focus on people’s personal ability to change by providing personal triggers.
This can be accomplished by accurately, unobtrusively and securely tracking a wider range of physiological parameters and by gathering contextual information on our behavior, habits, schedule, location, activity, etc. Combining detailed physiological data and detailed contextual data makes it possible to create an individual digital phenotype. This digital phenotype can then be used to give highly-personalized feedback and suggestions when you are open to act on them, urging you to eat healthy just when you are about to walk past the salad bar towards the fries, nudging you to take a break after a particularly stressful meeting, or suggesting a light snack just when your stress levels indicate that you are craving that cigarette. Compared to the generic advice now provided by wearables, this kind of personal feedback provided at the right time is a true paradigm shift.
In 2017, we already carried out a large-scale study that lays the foundation for a personalized digital stress coach, focusing on mental health and well-being. In this study, we did not only measure physiological stress signals, but we also evaluated self-reported stress and collected contextual information (via participants’ smartphones). Using wearable technology makes it possible to detect stress outside of the lab, in a real-life context. However, it also comes with new challenges. The data might be incomplete or subject to artifacts and we cannot control any of the context variables. E.g. did someone’s heart rate go up because he was experiencing stress or did he just run up a flight of stairs? For that reason, we are now developing objective quality indicators to determine when data is reliable enough to be included in the analysis. A second step will then be to develop advanced algorithms to mine these large, partially incomplete and unbalanced datasets.
Elena Smets (imec.ichange researcher and PhD student at KU Leuven) is working on imec’s SWEET study, which used wearable technology to collect the world’s largest dataset on stress detection.
The future of smart healthcare: disease interception
The grand challenge in smart health is disease interception: researchers are trying to establish the link between a disease and the medical factors that can predict it before any symptoms show. Wearable technology and Artificial Intelligence are two of the ingredients that are part of the solution. The first and foremost challenge will be rather mundane and practical: i.e. finding participants who are willing to commit to this study in the (very) long term – most likely years. A second challenge will be deciding which parameters we want to track, because we will only be able to establish what is relevant in hindsight. And then we need advanced data analytics to make sense of these vast amounts of heterogeneous (contextual, categorical, time series) data, blurred by real life’s interferences. This is only one part of a very complex puzzle though: we will need to connect this to other components of the human phenotype (stemming from genomics, proteomics and metabolomics, …) to properly understand the probability and causes of disease, and how a changing phenotype is related to disease emergence. Interception on individuals at risk is then expected through either pharmaceutical or non-pharmaceutical channels.
This new direction in smart health research will more than ever require a multidisciplinary approach. That is why – within the imec.ichange program – we aim to bring together different stakeholders, including not only technical partners (specialized in hardware or in data analysis), but also partners with medical expertise (hospitals, doctors, specialists, etc.) as well as coaching experts (psychiatrists, psychologists, behavioral scientists, etc.).
To develop truly smart healthcare solutions, we need to bring all these talented people – with their different fields of expertise – together with an open mind and a grand joint ambition.
At the end of this road, we should be able to truly quantify what it means to live a healthy lifestyle and how diseases can be intercepted. We may not quite have reached this goal by 2030, but we hope to do so in our lifetime, as it would have an impact beyond our wildest dreams.
Want to know more?
- Click here to download the MUSEIC V2 brochure.
- For more information on imec's research on stress detection, take a look at this press release.
- Read the related imec magazine articles: "Imec looking for partners to combat chronic diseases" (Imec Magazine, May 2017) and "It’s an illusion to think that everyone is interested in tracking their health" (Imec Magazine, September 2017)
Chris Van Hoof leads imec’s Connected Health Solutions R&D across 3 imec sites (Eindhoven, Leuven and Gent). Imec’s Connected Health Solutions teams provide solutions for chronic-disease patient monitoring and for preventive health through virtual coaching. Chris has taken wearable health from embryonic research to a business line serving international customers. Chris likes to make things that really work and apart from delivering industry-relevant qualified solutions to customers, his work has already resulted in 5 imec startups (4 in the healthcare domain). After receiving a PhD from the KU Leuven in 1992 in collaboration with imec, Chris has held positions as manager and director in diverse fields (sensors, imagers, 3D integration, MEMS, energy harvesting, body area networks, biomedical electronics, wearable health). He has published over 600 papers in journals and conference proceedings and has given over 100 invited talks. He is full professor at KU Leuven.
Published on:
15 December 2017