Monitoring for diagnosis and follow-up of respiratory conditions (e.g. chronic obstructive pulmonary disease (COPD), asthma, pulmonary fibrosis) is based on questionnaires, and obtrusive tools and measurement techniques such as spirometry. Imec proposes a new approach to make respiratory monitoring more patient-friendly and continuous. It includes sensing new modalities in user-friendly form factors (such as wristbands and patches) and combining the measured data with advanced algorithms in clinically validated studies. This will allow medical device companies to introduce continuous respiratory monitoring in hospitals and in patients’ daily lives. Also, it will enable pharma companies to gather real-world-evidence data to prove whether current treatments are effective, and to better screen populations for potential abnormalities.
Compared to cardiac monitoring, the respiratory monitoring field has gained less attention and has witnessed fewer technological innovations both in consumer and medical applications. Can the COVID-19 pandemic put respiratory monitoring higher on the agenda of medical device and pharma companies and push new developments forward?
Carlos Agell, program manager Connected Health Solutions at imec: “A good wearable platform for respiratory monitoring would be a big step forward for patients suffering from diseases such as COPD and asthma.
Whether wearable devices can also be used for viral or bacterial infections affecting the respiratory track (such as the current COVID-19 pandemic), remains to be seen. What is clear however, is that pervasive respiratory monitoring systems allow to collect objective data while people are staying at home, not infecting others, and, if necessary, over a long period of time.
Wearables could act as an early warning system of one’s changing condition. In this perspective, a wearable patch tracking one’s breathing parameters or blood oxygen saturation, could be one of the building blocks of a strategy towards dealing with future pandemics.”
And where pandemics are hopefully temporary, many respiratory diseases are chronic problems, affecting patients’ everyday lives. Just think of the enormous burden of exacerbations for COPD patients and nocturnal asthma attacks for children. Also, the fact that millions of people are suffering from these conditions, has an enormous effect on the economy. Therefore, new monitoring technology and better treatments are vital.
Today’s situation: from questionnaires to intermittent tests
Today, hospitals rely on several standardized tests to check patients with respiratory problems such as COPD, pulmonary fibrosis, cystic fibrosis and asthma, whether for diagnosis or follow-up of the disease and treatment plan.
- Spirometry is the most common pulmonary function test. It measures the amount and speed of air that can be inhaled and exhaled. It requires the patient to breathe through a device (which is neither practical nor continuous).
- Pulse oximetry monitors the oxygen saturation of a patient's blood. It requires wearing a finger clip, which is unsuited as a long-term monitoring solution outside a clinical setting.
- Lung scans can help in diagnosing certain lung problems. But they can only be done at a hospital facility and require specialized equipment and trained technicians.
Carlos Agell: “The disadvantages of many of these tests are that they need to be executed by well-trained professionals, often don’t allow for continuous monitoring and are frequently uncomfortable for the patient.
And how is the patient doing outside the hospital, in his or her home environment? For this information, the doctor must rely on questionnaires. In general, patients underestimate their condition or just don’t remember how they were feeling a week or a month ago. Follow-up consults would therefore benefit a lot from objective data, measured during a patient’s daily life.”
And although there are many positive evolutions, such as ‘digital assistants’ keeping an eye on the patients at home (such as Luscii for COPD patients and other telemedicine applications), there is still a lot that can be done to improve the monitoring of patients, especially outside the hospital.
The disadvantage of today's standardized tests is that they need to be executes by well-trained professionals, often don't allow for continuous monitoring and are frequently uncomfortable for the patient. We believe that wearable technology can be used as a complementary tool to monitor patients at home. Our recent study on COPD patients shows the potential of wearable technology for these patients.
A multidisciplinary approach is key to innovate respiratory monitoring
For more than 15 years, imec has been researching wearable devices to monitor health parameters. Carlos Agell: “With a background in electronics, our first focus was on chip design and system integration, low-power processing and wireless communication. Today, we combine this with algorithm development and machine learning, and – together with clinical partners – we set up small-scale trials with patients to validate systems and algorithms, and to identify novel applications and system requirements.
We strongly believe that any new technology based on novel biomarkers needs to be scientifically validated. Hereto, we partner with healthcare institutions and publish the research outcome in state-of-the-art scientific publications and conference proceedings.
We perform this research with a team of about 60 researchers with expertise ranging from chip design to algorithm development, biomedicine and data science. It’s this unique range of competences that has resulted in impressive results and numerous scientific publications, as well as successful collaborations with industry (e.g. BioTelemetry, Samsung, ...) and clinical partners (ZOL, Radboud University, ...). We aim to be a one-stop-shop for medical device and pharmaceutical companies to do joint research on specific building blocks or complete applications, or to license some of our hardware or software Over the years, we have gathered a lot of expertise in many application domains (stress management, heart failure, epilepsy, ...). Respiratory monitoring is high on our research agenda, mainly because we believe there is a lot to gain here, both for the industry and the patients.”
An example of this multidisciplinary approach: wearable and continuous monitoring of COPD patients
PATIENT STUDY
In a recent study together with the biomedical signal processing and interpretation (BIOSPIN) group at the institute for bioengineering of Catalonia (IBEC) and the department of respiratory medicine at Ziekenhuis Oost-Limburg (ZOL), a respiratory sensing technology was tested on COPD patients. Willemijn Groenendaal, principal scientist at imec: “COPD is a leading cause of death worldwide. The current diagnosis of COPD and the assessment of its severity requires a spirometry test, complemented with information from questionnaires. The interval of these tests and the subjectivity of the questionnaires is not ideal for the complex clinical condition of COPD patients.
Imec, as well as other research groups, have shown the potential of thoracic bioimpedance and electromyography measurements as more comfortable and less invasive methods. For the first time, we conducted a trial with COPD patients, combining the analysis of bioimpedance and myographic measurements, to prove its applicability for unobtrusive respiratory monitoring.”
In the clinical setting of the hospital, the research partners used a.o. a wearable research prototype device developed by imec to measure bioimpedance, complemented by a desktop device to determine muscle signals (electromyography and mechanomyography). In the future, all these measurements could be combined into one wearable device. The aim of this study was first to explore the potential of these signals for COPD patients.
Carlos Agell: “We have developed four investigational devices that we use in our patient studies as a 24/7 data collection platform. These include patch and wristband form factors. And they allow us to collect raw data in a user-friendly way and even in the real world, while patients and users carry on with their daily activities. A great example of such a real-world trial was our SWEET study on stress detection in 2018, collecting the world’s largest data set on stress.”

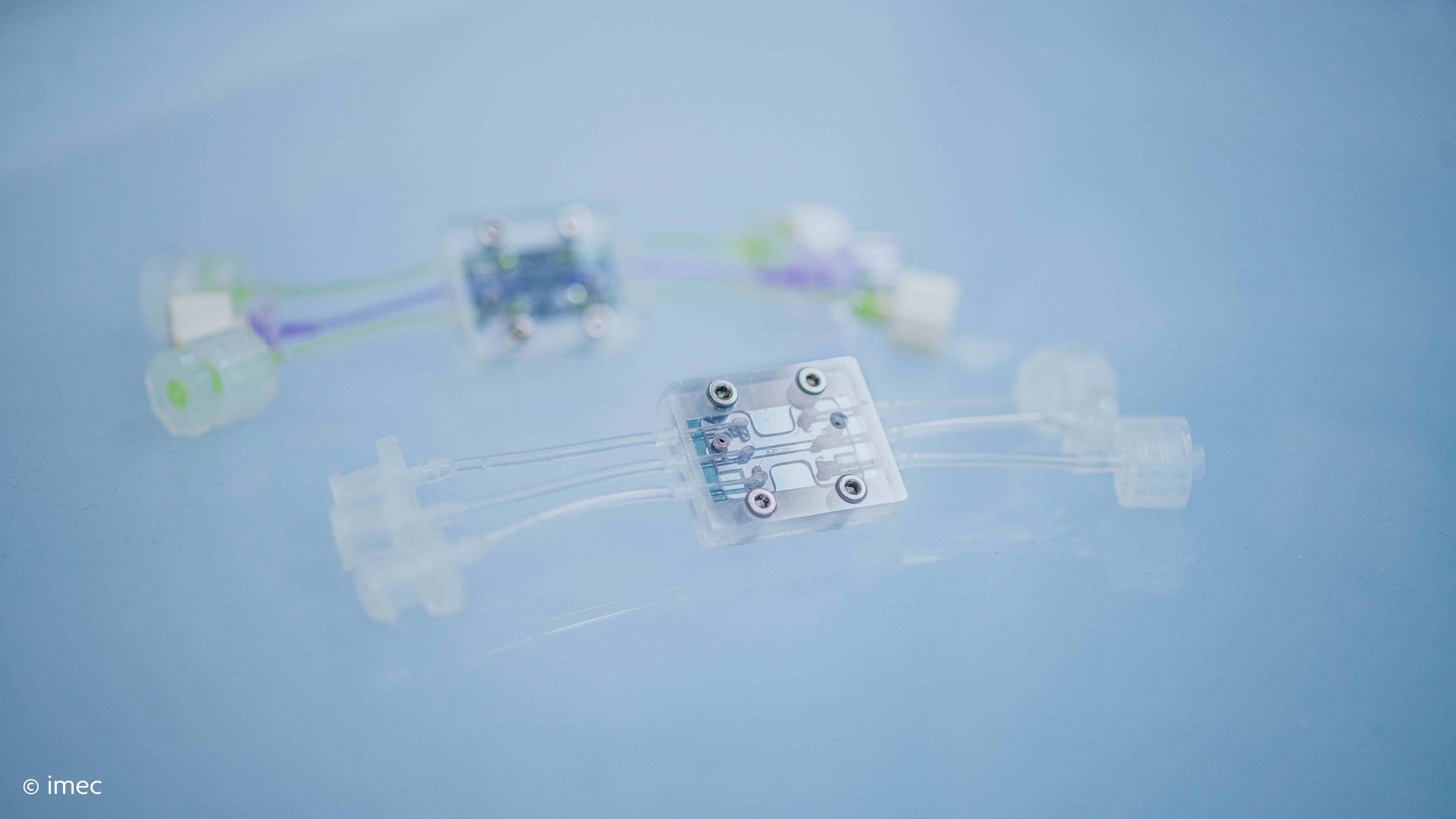
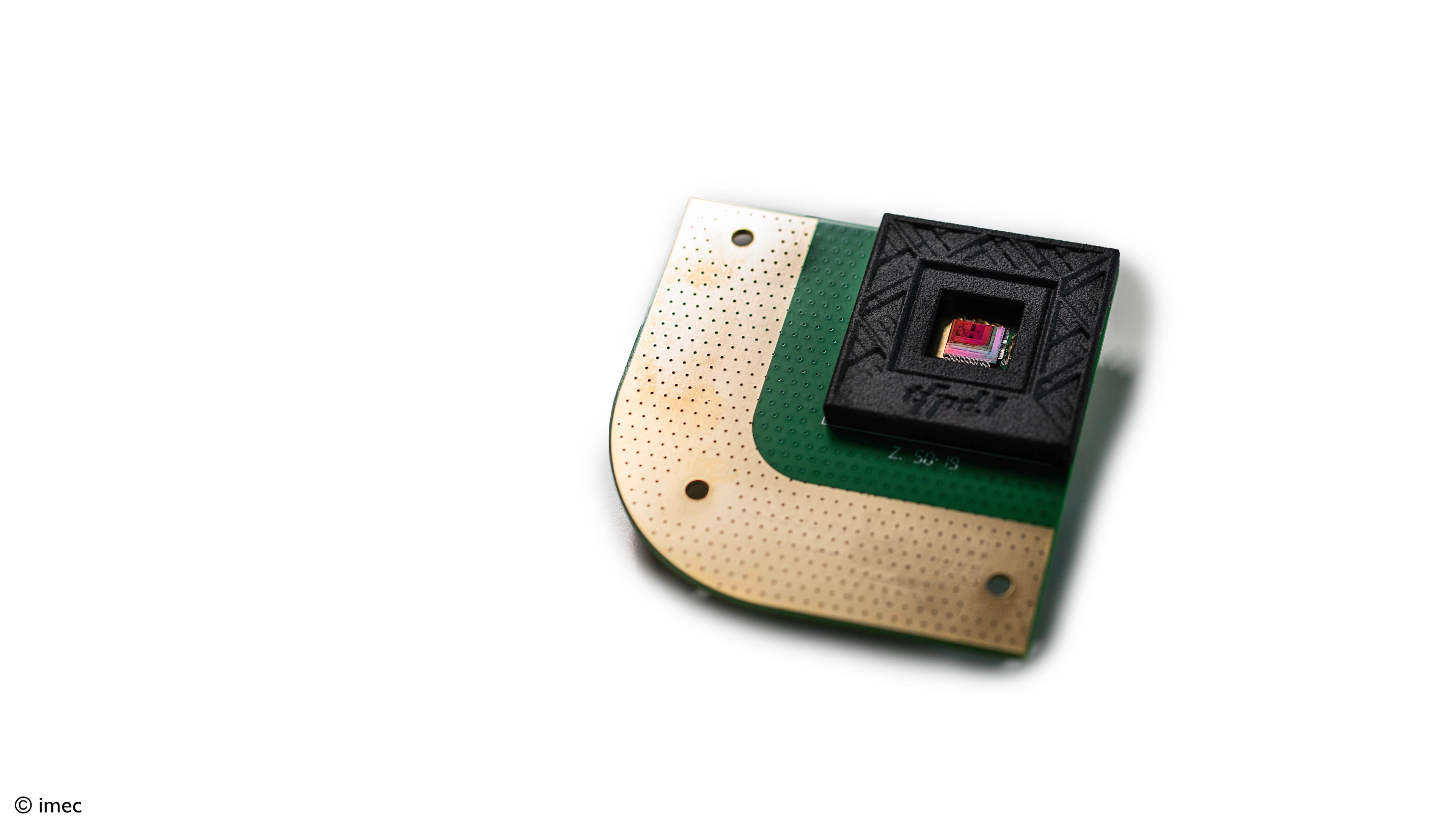
Imec’s investigational devices enabling data collection in clinical settings or in real-world surroundings, including patch and wrist form factors, from left to right: health patch disposable & comfortable device, Nightingale re-usable & flexible multi signal device, Chill+ mental health platform, cardio watch for cardiac monitoring.
ALGORITHM DEVELOPMENT
From the COPD patients, data were acquired using imec’s research device and a standard wired acquisition system. Next, algorithms were developed to make sense of these data. Willemijn Groenendaal: “Typically, we develop 3 kinds of algorithms:
- Signal-level algorithms. Sizeable algorithmic effort goes towards telling apart clean usable signals from unusable and distorted ones. For example, data that are acquired while the patient is still, are much more trustworthy than when under severe motion. Therefore, we develop signal quality indicator algorithms, gating the execution of other algorithms. For the specific case of COPD patients, this concerned the signal quality of the bioimpedance, electromyography and mechanomyography sensors.
- Digital-biomarker-level algorithms. Next, we do feature extraction, which focuses on extracting information from one or several physiological systems. For instance, heart rate is a feature extracted from the ECG signal. We develop algorithms to calculate – e.g. in case of the COPD patients – inspiratory time, duty cycle, respiratory frequency and inspiratory volume. At this level though, the features only portray a partial view on the patient’s status.
- Application-level algorithms. At this level, we combine data from multiple biomarkers, physiological systems and body-subsystems (heart, respiration, exercise, ...) to make decisions on the specific disease. For the COPD study for example, we were able to classify the patients in three ‘severity’ groups based on novel combinations of the bioimpedance and myography parameters. These novel indices could one day be used to monitor, in a continuous way, the progress of the disease, at the patient’s home. Of course, further studies and developments are needed.
For the second and third level, we use artificial intelligence. We thereby focus on explainable or white-box AI because we believe that physicians must be able to understand why the system makes a certain decision, to be able to intervene when necessary. Therefore, it is essential to also have biomedical experts in our team and to have collaborations with clinical partners, complementing the algorithm developers.”

Three kinds of algorithms are essential for truly reliable and smart wearable monitoring systems. In this scheme, the three levels that were worked out for the COPD use case, are shown.
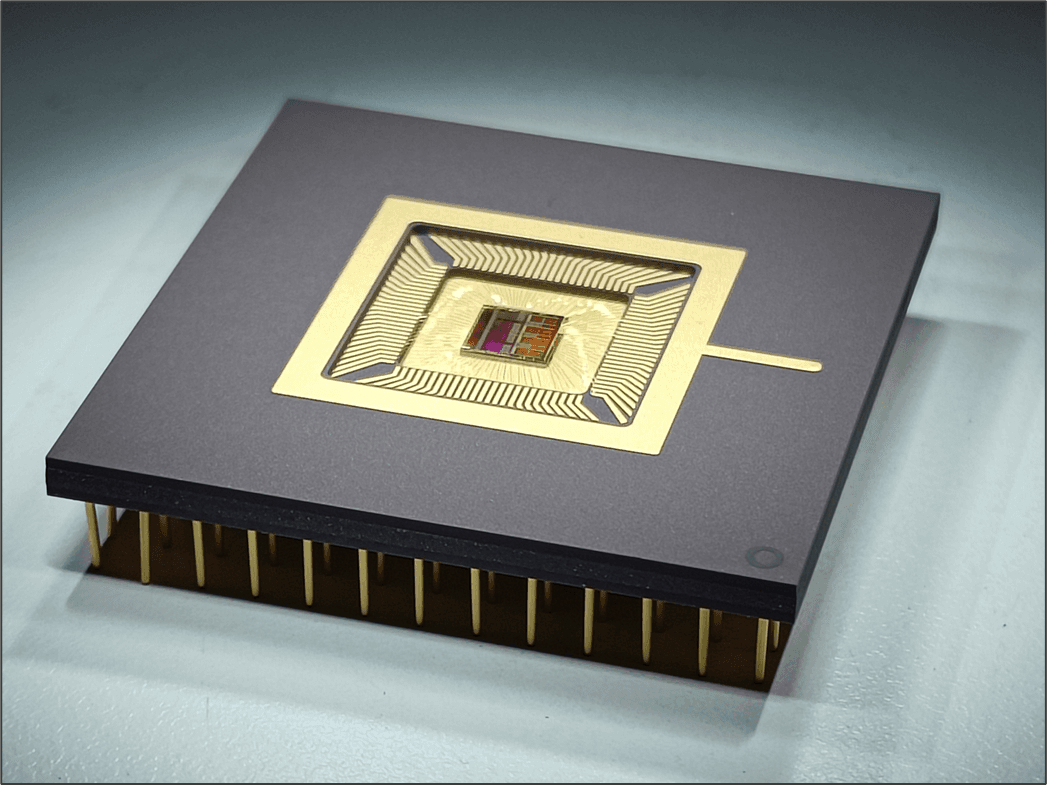
CHIP AND SYSTEM DESIGN
In order to develop truly compact and comfortable wearable monitoring devices, chip and system design are also key. As it happens, this is one of the core businesses of imec. Carlos Agell: “At the heart of our wearable health platform is a fully integrated battery-powered wireless sensor hub. It can measure multiple parameters simultaneously (ECG, PPG, BioZ, ...) while consuming very little power (important for continuous monitoring mode) and with a high level of security.
The form factor in which to package these respiratory sensors is flexible. It can be a patch (disposable or reusable), a chest belt, a necklace or a sensor shirt. The sensors can even be integrated in a mattress, office chair or car seat. It all depends on the specific application. The general rule is that it should be comfortable for the patient, in order to guarantee compliance.”
Conclusion & future vision
With this holistic approach, it is possible to develop wearable monitoring technology for objective, continuous and non-invasive data collection. Wearables promise a better future for respiratory patients, in different ways:
- Provide specialists with continuous data when patients are moving from the hospital to the home setting, to keep a close eye during this critical timeframe. This could allow to shorten the hospital stay.
- Supply doctors with objective and reliable data from the patient’s time at home, to consult during follow-up consultations.
- Monitor patients at home to alert their specialist when the patient’s condition is deteriorating, and this in a very early stage.
- Screen more people for their respiratory condition and use these data – in combination with other measurements and the doctor’s expertise – to also diagnose mild conditions of a respiratory disease.
- Use in clinical trials to evaluate drug efficacy, both in classical Randomized Control Trials and in Real World conditions.
- Detect drug efficacy in single patients when a treatment plan is being set up.
Carlos Agell: “Wearable sensory devices today are more reliable, more intelligent and easier to use than their predecessors. They can therefore be used in studies to gain further insights in digital biomarkers for certain diseases. Maybe, one day, respiration characteristics can be combined with other vital sign characteristics, to give an indication of stress or pain levels in certain patients, or to detect the general wellbeing of e.g. cancer patients or people suffering from depression. Its use will be widespread, and the possibilities are enormous.
Thanks to the developments in electronics and algorithms, and with the help of patient studies, now is the time to develop, manufacture and use these promising solutions and improve the life of many patients”
Want to know more?
- Would you like to discuss your idea or collaborate with us? Please contact Zohaib Gulzar, Business Development Manager at imec. Here, you can find information on our collaboration models.
- Would like to dive into more technical details of the COPD study described in this paper? Use this link to access this Transactions on Biomedical Engineering paper. Also, browse through the scientific papers on our webpages on technology for respiratory care. Below each page is a list of publications.
- On June 4 and July 8,2020 imec hosted a webinar on respectively vital sign monitoring and respiratory monitoring. Feel free to ask for the recordings.
- Get a nice overview of imec’s connected health solutions.
- Learn more about imec.

Carlos Agell is Program Manager at imec. He has a background in wearable device development, having taken leadership roles in developing two FDA-approved medical devices in the field of wearable cardiology. He oversees the development of connected health solutions projects and sets strategy directions for research topics within the department, which includes work in multiple therapeutic areas, including respiration. He is member of the Dutch chapter of the standardization committee for medical devices, which develops next-generation international standards in the field.

Willemijn Groenendaal is a principal scientist at imec, where she leads research activities with a focus on wearable monitoring and algorithms in the clinical domain. She is involved in studies with patients suffering from COPD (Chronic Obstructive Pulmonary Disease), sleep apnea, and heart failure. These studies are done in close collaboration with hospitals.
Willemijn Groenendaal received her master’s and Ph.D. degrees from the Eindhoven University of Technology, Eindhoven, The Netherlands, in 2006 and 2011, respectively. She has been a Postdoctoral Associate with the Weill Cornell Medical College, New York, NY, USA.
Published on:
13 May 2020