Your blood tells a story
When we hear the word ‘biopsy’, we immediately tend to think of a minor procedure in which a small piece of tissue is removed from the patient for further investigation. But a ‘liquid biopsy’ is less invasive than a surgical biopsy. In fact, a liquid biopsy usually involves just taking a blood sample, although a urine or saliva sample also falls into the same category.
Liesbet Lagae: “Cancer specialists have discovered that the blood of cancer patients differs from the blood of healthy people. As a result, oncologists are able to detect all kinds of indications in this ‘different’ blood that can help with the diagnosis and treatment of cancer.”
“For instance, they may find tumor cells in the blood that have separated from the original tumor (that may be located in the lung tissue, for example). They are called ‘circulating tumor cells’, or CTCs. Another area of interest in the blood sample is blood platelets. We now know that the blood platelets in cancer patients are different from those in someone healthy. What the tumor appears to do is use the blood platelets to help itself grow. Phospholipids in the blood also contain information about cancer. For instance, determining the profile of the phospholipids present makes it possible to discover prostate cancer in the blood.”
Just why there are all these differences between 'healthy' and 'cancer' blood is still a mystery in the main. Shedding more light on this mystery, will help cancer experts to gain a greater insight into exactly how cancer goes to work in our body.
Why use a liquid biopsy?
A liquid biopsy has several benefits in comparison with a tissue biopsy: for a start, it is less invasive for the patient and it can be carried out as often as necessary, which makes it possible to track the patient’s progress better through the treatment process. The liquid biopsy also provides a ‘live’ picture of the cancer at that specific moment and there is never a problem in terms of being able to take the biopsy (for example when the patient is too weak to undergo a tissue biopsy, or if the primary tumor is difficult to reach).
Yet despite all these advantages, liquid biopsies will never be the only technique used. That’s because cancer is a highly complex disease and for doctors to obtain a full picture of the situation, various techniques need to be used alongside each other – liquid and tissue biopsies, imaging. Liesbet Lagae: “For example, we can see that the cancer cells in the blood often have properties that differ from the cancer cells in the original tumor. The tumor may also be made up of different types of cells (called a ‘heterogeneous’ tumor). This makes the liquid biopsy a welcome and excellent new adjunct in the toolbox of cancer specialists, in addition to tissue biopsies and imaging.”

“In the future, it will be possible to use a blood sample to obtain a faster diagnosis of cancer. It will also enable us to determine the best type of treatment and to monitor how the treatment is progressing. This will help doctors to predict the tumor’s resistance to certain types of drugs, as well as to detect metastases more quickly and also to conduct regular checks into the genetic material of the tumor.”
A well-known example of ‘determining the best treatment’ can be found in breast cancer. Specifically, there are certain types of breast cancer that can be treated well with a hormone treatment, with little chance of relapse or the tumor spreading. To determine whether the patient has this particular type of breast cancer, the receptors present in the tumor cells are examined. This is a fairly expensive treatment and so the doctor needs to be sure that the patient will actually benefit from the therapy.
At the moment, this hormone treatment can only begin once a tissue biopsy or operation has demonstrated that the tumor has these specific receptors. Both from an economic and a medical point of view, liquid biopsies may be of great value in these cases because it means that the treatment can start more quickly.
Another example that is already being used today is determining the resistance of tumors in patients with lung cancer. Often resistance doesn’t occur until after 10 months of treatment using EGFR-targeted therapy. If the doctor can determine that resistance in the blood, he or she will then switch to another drug, in this case osimertinib.
The possibilities offered by liquid biopsies are enormous, although a great deal of research is still required to enable the correct interpretations to be made of the values measured in the blood.
Making the liquid biopsy ‘digital’
Today, it requires large and expensive tools and highly qualified staff to perform the liquid biopsies. Chip technology and nanotechnology can be used to make liquid biopsies easier and more user-friendly. Imagine that doctors in the future will have disposable cartridges that they can use to analyze a drop of their patient’s blood in a compact device that screens the blood for DNA, cells, phospholipids, etc. This will then tell them more about whether or not there is cancer present, the type of tumor, etc. – plus the analysis can be carried out several times throughout the patient’s treatment.
The main benefit of the evolution from tissue biopsy to liquid biopsy and then on to digital liquid biopsy will be that the liquid biopsy (e.g. for cancer patients) will become much faster and easier to carry out.
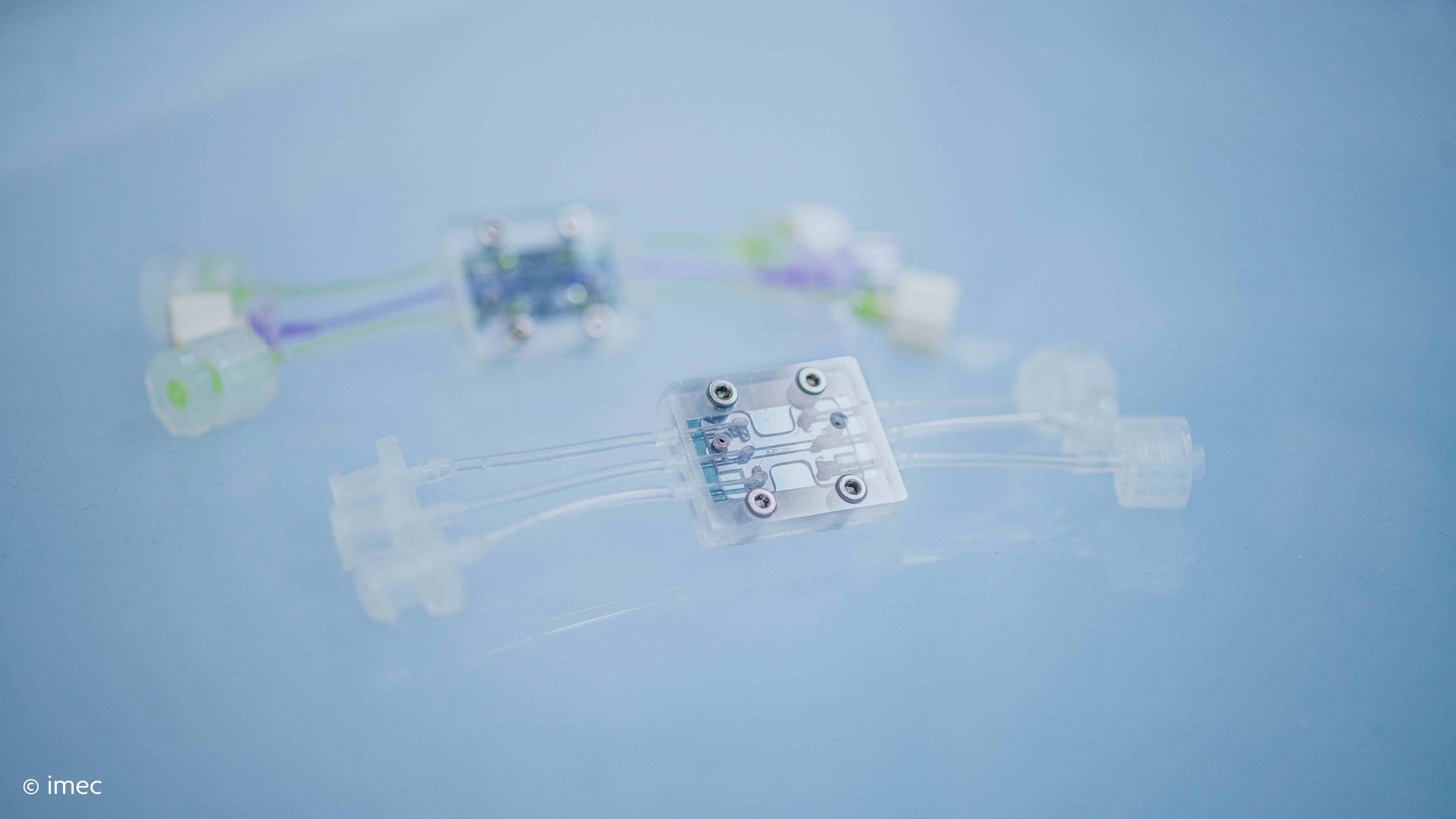
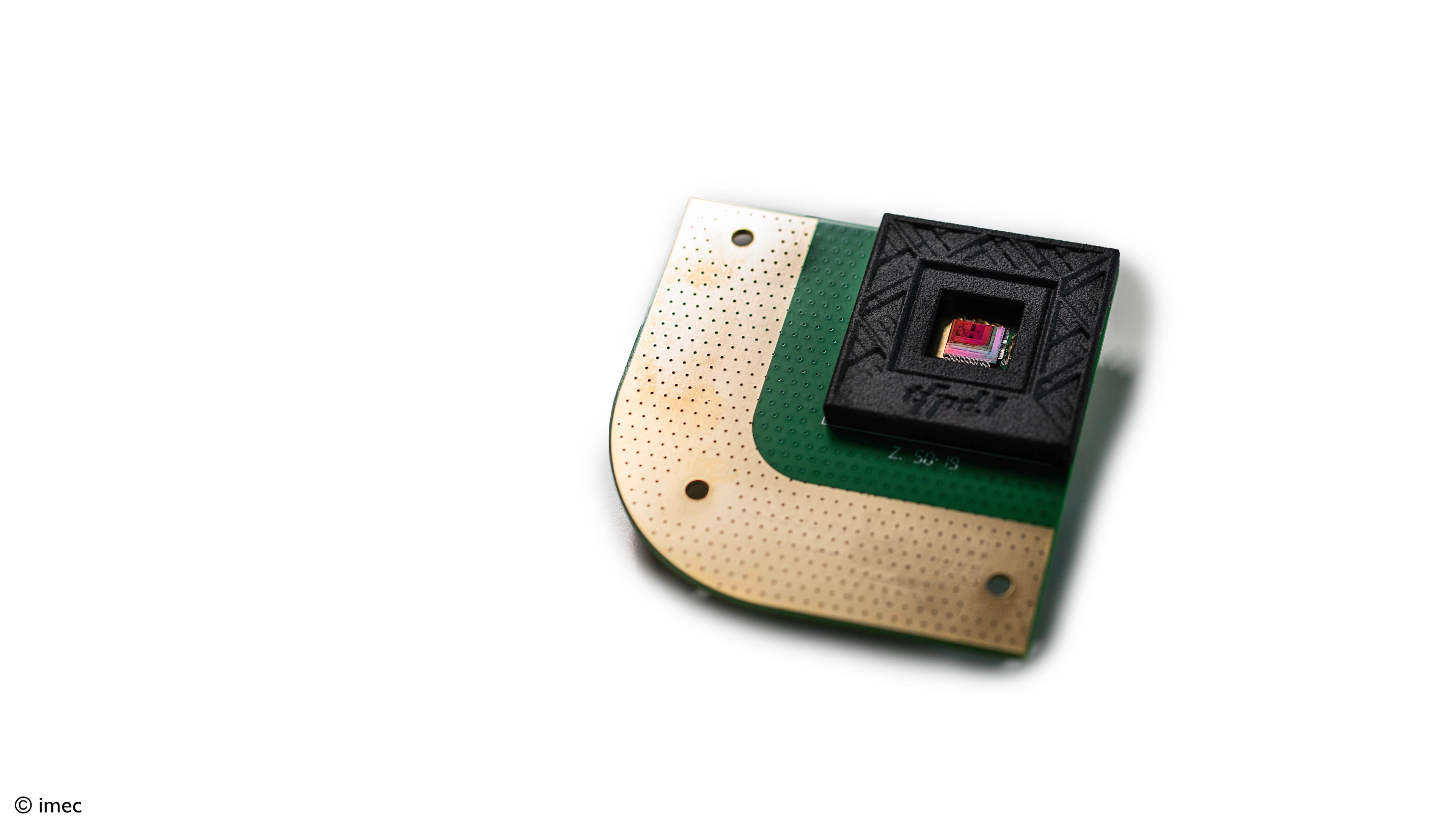
Liesbet Lagae: “At imec we are working on a technology platform that can be used for digital liquid biopsies. By combining electronics, sensors, photonics and microfluidics, we have all the building blocks to produce a cartridge of the type described above, which means that it will be very easy to carry out liquid biopsies in patients.”
The technology platform being developed by imec can be used for digital liquid biopsies.
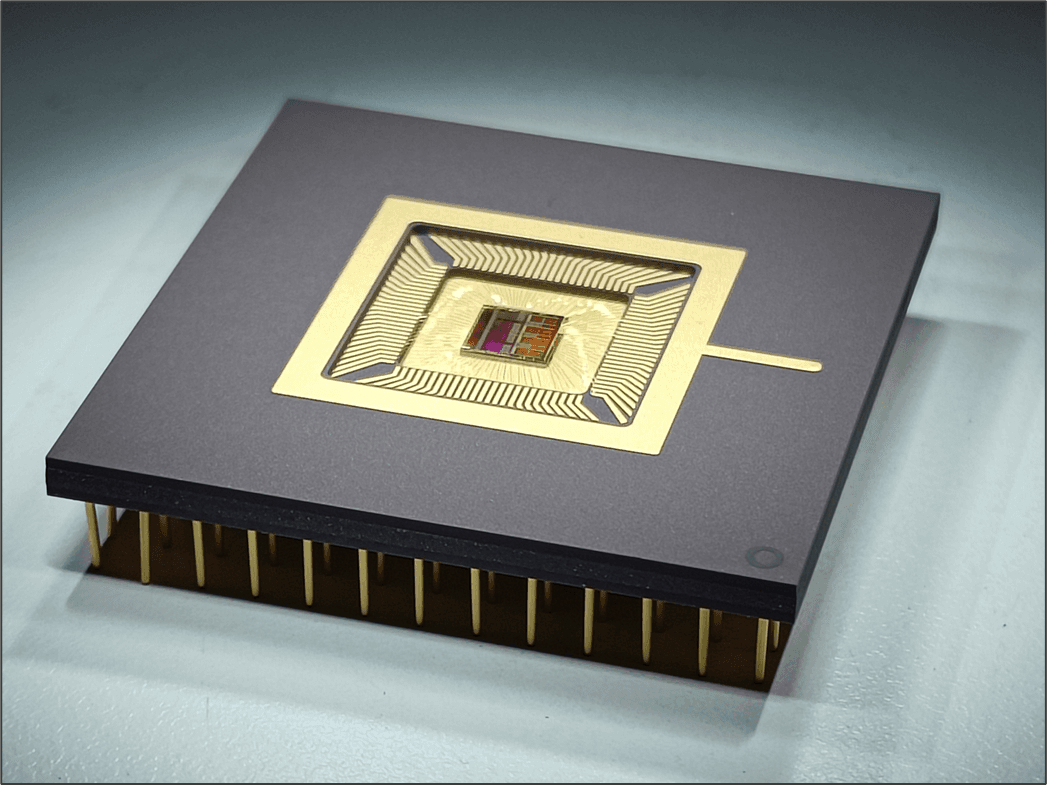
“Two of the components that we produce clearly demonstrate the power of nanotechnology and the integration capabilities inherent in electronics. The first of these is the lens-free microscope. Cells flow along a microfluidic channel where they are illuminated from above by a laser. The light is captured below by an image sensor, while software enables an image of the cell to be reconstructed. Various types of cell can be identified in this way without using (fluorescent) labels.”
Imec has shown that it is possible, using its lens-free microscope technology, to make a distinction between the various types of cells in the blood, and tumor cells. These tests were conducted in conjunction with the Frederik De Smet laboratory, Translational Cell and Tissue Research, KU Leuven
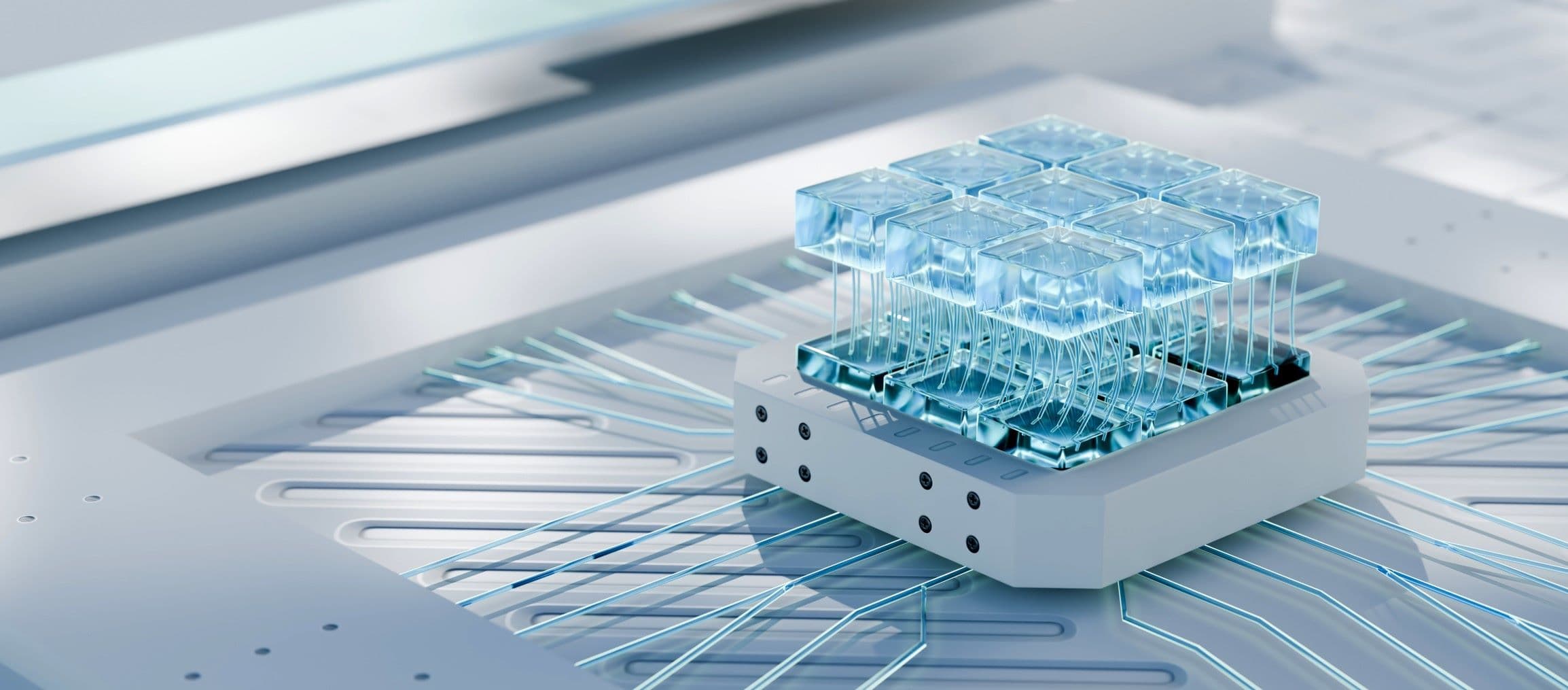
Another important building block in the imec technology platform is a cell-sorting technique based on a thermal bubble switch. That is because when a certain type of cell is identified, it is important to isolate it from the other cell types. Liesbet Lagae: “This is done by switching on mini heating elements above the microfluidic channels in which the cells are moving. This creates little gas bubbles that push the cells in a particular direction. As a result, various types of cells can be sorted in different microfluidic channels.”
This technique is twice as fast as current techniques (5000 cells can be sorted per second). This number can also be increased enormously when different channels are used alongside each other. Another important factor is that this is a non-destructive technique, which means that the isolated cells can be examined even more closely after the sorting process is complete.
With the thermal bubble switch, 5000 cells can be sorted per second in microfluidic channels. This architecture can be easily upscaled, with hundreds of these channels operating next to each other, resulting in an enormous output.
Can we outwit cancer?
It is, of course, good news that cancer specialists now have a new tool in liquid biopsies to fight cancer (and that electronics experts can help them to do so). But (digital) liquid biopsies are no silver bullet.
Liesbet Lagae: “If you were to be told today that you have cancer, a number of different treatments are possible: the tumor can be removed by an operation or treated by chemo-, radio-, hormone- or immunotherapy. A liquid biopsy may help you to determine better which form of treatment has the best chance of success, as well as whether and when any resistance is likely to occur. But it is just as important for cancer experts to gain more insight into the way the cancer works and to keep on developing new, more effective treatments. In the end, all these pieces of the puzzle will enable us to outwit cancer. And as an electronics person, I am delighted to be able to make my own small contribution.”
The Leuven Cancer Institute
Leuven Cancer Institute, or LKI, is where doctors, health care providers and researchers from University Hospital Leuven and KU Leuven all come together in their fight against cancer. Their great strength lies in combining research, treatment and care so that every available weapon can be geared with the others to provide maximum effectiveness. LKI is where targeted projects using innovative technology are devised right across the full spectrum of cancer types.
Want to know more?
- If you would like more in-depth technical information about imec’s lens-free microscope or the thermal bubble switch, you can ask to receive scientific papers by sending an e-mail to imecmagazine@imec.be

Liesbet Lagae is co-founder and currently Program Director of the Life Science Technologies in imec. In this role, she oversees the emerging R&D, the public funded activities and early business creation. She holds a PhD degree from the KU Leuven, Belgium for her work on Magnetic Random Access Memories obtained under an IWT grant. As a young group leader, she has initiated the field of molecular and cellular biochips leveraging silicon technologies at IMEC, Belgium. The life science program has grown from emerging activities to a mature business line that provides smart silicon chip solutions to the life science industry. Applications include medical diagnostics, point-of-care solutions, DNA sequencing, cytometry, bioreactors, neuroprobes, implants. She holds a prestigious ERC consolidator grant for developing a platform on single cell analysis and sorting. She has (co-) authored 125 peer-reviewed papers in international journals and holds 15 patents in the field. She is also part-time professor in nanobiotechnology at KU Leuven/Physics department.
Published on:
27 September 2017